Изгледа дека сте во САД
Имаме различна локација (www.q-bital.com) која подобро одговара на вашата локација
Заостанатиот број на пациенти кои чекаат повеќе од шест недели за ендоскопија значително се зголеми од почетокот на пандемијата Ковид-19, а листите на чекање сега треба итно да се решат. А неодамна објавен извештај од NHS Англија, повикува на реформи и предлага воведување мрежа на дијагностички центри во заедницата, од кои некои ќе содржат капацитети за ендоскопија.
А мобилна или модуларна ендоскопија единицата може да се користи привремено, или заедно со центар на заедницата, за да се создаде самостоен објект кој обезбедува посебна патека за изборни услуги за ендоскопија. Итна потреба да се реши времето на чекање Побарувачката за ендоскопија значително порасна во текот на изминатите пет години, и иако активноста се зголеми, времето на чекање се зголеми побрзо, што предизвикува заостанување. Процедурите на флексибилна сигмоидоскопија забележаа највисоки стапки на раст, главно поради отпочнувањето на програмата за скрининг на дебелото црево.
За време на Ковид-19, потребата за длабинско чистење на опремата и објектите меѓу пациентите доведе до пад на продуктивноста и откажани процедури и, како резултат на тоа, повисоки и подолги чекања. Севкупно, нивоата на активност на ендоскопијата се намалија за над 90% на врвот на пандемијата.
Итни ендоскопски процедури на врвот на пандемијата беа преземени секаде каде што беше можно во операционите сали со негативен воздушен притисок. Гастроскопијата, исто така, првично беше означена како процедура за генерирање аеросоли (AGP), која носи ризик за ендоскопите ако пациентите се позитивни на Covid-19 или не се сигурни за Covid-19, но гастроскопијата повеќе не се смета за AGP под водство на PHE.
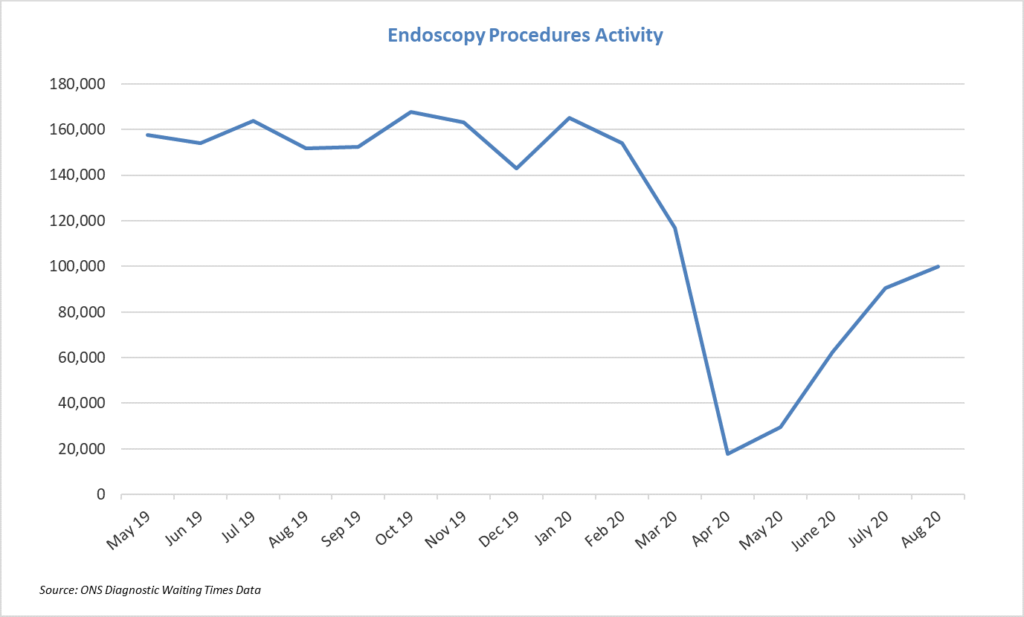 Најновите бројки од NHS Англија покажуваат дека иако активноста на ендоскопијата е значително зголемена од април, стапката на закрепнување е значително забавена. Активноста во август беше околу две третини од таа во нормален месец. Ова, во комбинација со фактот дека списоците на чекање не се значително зголемени во август, и покрај ниското ниво на активност, сугерира дека сè уште постои значителен „скриен“ заостаток на луѓе кои сè уште не се запишале на листите на чекање.
Потребата за докажување во иднина
Сега има итна потреба да се воспостават минимални капацитети за ендоскопија „Ковид-19“ за да се помогне закрепнувањето. Извештајот признава дека пристапот до опремата и капацитетите за ендоскопија, особено оние за колоноскопија, веќе биле под значителен притисок пред пандемијата. Како и ограничувањата на работната сила, програмата Get it Right First Time (GIRFT), исто така, откри дека околу 20 трустови на NHS најверојатно ќе бараат целосна обнова на нивните ендоскопски капацитети со други на кои им треба подобрување.
Најновите бројки од NHS Англија покажуваат дека иако активноста на ендоскопијата е значително зголемена од април, стапката на закрепнување е значително забавена. Активноста во август беше околу две третини од таа во нормален месец. Ова, во комбинација со фактот дека списоците на чекање не се значително зголемени во август, и покрај ниското ниво на активност, сугерира дека сè уште постои значителен „скриен“ заостаток на луѓе кои сè уште не се запишале на листите на чекање.
Потребата за докажување во иднина
Сега има итна потреба да се воспостават минимални капацитети за ендоскопија „Ковид-19“ за да се помогне закрепнувањето. Извештајот признава дека пристапот до опремата и капацитетите за ендоскопија, особено оние за колоноскопија, веќе биле под значителен притисок пред пандемијата. Како и ограничувањата на работната сила, програмата Get it Right First Time (GIRFT), исто така, откри дека околу 20 трустови на NHS најверојатно ќе бараат целосна обнова на нивните ендоскопски капацитети со други на кои им треба подобрување.
Во извештајот на NHS Англија, се проценува дека се потребни околу 200 нови простории за ендоскопија во NHS Trusts за да се покрие тековниот раст на ендоскопијата и да се овозможат планираните проширувања на програмата за скрининг на дебелото црево. Потребни се и нови единици за деконтаминација за ендоскопија, а во извештајот се препорачува и замена на целата постоечка опрема за снимање постара од 10 години.
За жал, не постои национален регистар на средства за установи за ендоскопија, а во извештајот се препорачува итно да се спроведат истражувања за опремата/објектите и персоналот за да се олесни и краткорочното и долгорочното планирање. Извештајот сугерира учество во Националната база на податоци за ендоскопија (NED) од страна на 20% на NHS Trusts кои веќе не го прават тоа.
Извештај објавен од Public Policy Projects во партнерство со Vanguard Пред две години, покажа дека повеќе од една третина од болниците работат со комплети за деконтаминација за ендоскопија со опрема што ги приближува или ги надминува препораките на производителите и дека околу 251 TP4T болници имаат комплети за деконтаминација за ендоскопија стари повеќе од десет години. Практично решение за ендоскопија Се надеваме дека воспоставувањето на установи за ендоскопија без КОВИД во некои од предложените центри за дијагностичка заедница или едношалтерските продавници , заедно со тестирањето и на пациентите и на персоналот пред сите процедури, може да значи дека барањето за длабинско чистење меѓу пациентите ќе биде значително намалено, што ќе овозможи пропусната моќ да се зголеми поблиску до нормалните нивоа. Пациентите кои се позитивни на Ковид-19 и оние на кои им е потребна итна ендоскопија пред да се утврди статусот на Ковид-19, треба да продолжат да ги прават нивните процедури во установи со негативен воздушен притисок (обично операциони сали).
Што се однесува до работната сила, извештајот препорачува формирање академии за обука за да се зголеми бројот на немедицински колоноскописти и да се овозможат постоечките колоноскописти да преземат скрининг колоноскопија. Ќе бидат потребни и повеќе медицински сестри за ендоскопија за да се задоволи дополнителната побарувачка.
Без инвестиции или реформирано доставување услуги, со сопствен прием, NHS ризикува да не може да ги исполни целите, вклучително и амбицијата да се дијагностицира 75% на луѓе со рак во рана фаза и да се подобрат резултатите на пациентите. Дури и ако плановите бидат брзо одобрени, препораките во извештајот ќе бараат време за да се спроведат. Но, со оглед на тоа што заостатокот расте секој месец, дали чекањето е опција?
За секој месец што е загрозена продуктивноста, листата на чекање расте над нивото што може лесно да се врати без да се надмине 100% од постоечкиот капацитет. Потребно е привремено решение и флексибилна клиничка инфраструктура може да го даде одговорот. Мобилните и модуларните единици за ендоскопија може да се комбинираат со флексибилни единици за контаминација на ендоскопија и да се постават на речиси секоја локација - во непосредна близина на дијагностички центар или на друго место во заедницата - за да се создаде самостојна локација без Covid за изборна ендоскопија.
Прочитајте го извештајот, кој вклучува детален преглед на ендоскопската активност, овде .
Копија од извештајот „Гледајќи внатре: Состојбата на ендоскопијата во Англија“ , произведен од Public Policy Projects во партнерство со Vanguard, може да се побара од контактирање со нас .


Vanguard здравствени решенија
Unit 1144 Regent Court, The Square, Gloucester Business Park, Gloucester, GL3 4AD

Имаме различна локација (www.q-bital.com) која подобро одговара на вашата локација